This is a guest post / repost from Smart Money, MD on the topic of whether going to a highly-ranked medical school matters:
Some of us are overachievers. Some of us are overachieving doctors. What if you’re in-between? Let’s say that you’re an overachiever, and you want to become a doctor.
Should you go all the way up top and get that medical degree from a top private institution? Does it even matter? With tuition costs skyrocketing, you can easily spend $60,000 annually on tuition alone for each year in medical school. Add another $10-$15k in room and board, and you will be about a quarter million in the hole by the time you get out. In contrast, medical school tuition in 2016 for UT Houston for in-state resident is only about $20,000 annually. That’s a big difference.
These are considerations that are rarely taught or even discussed. If you are planning to go to medical school, it does pay to consider the consequences thoroughly before you proceed.
Does a prestigious degree help get you a better job?
It depends. It depends on where you plan to work. In clinical medicine, you can either work at an academic institution or in the private sector. Many job situations in the academic world require teaching, research, or involvement in administration. If I were a departmental chair looking to bring on a clinician-researcher, I’d want someone who not only can practice medicine well, but also has strong writing skills, coherent presentation abilities, and innovative characteristics. If two candidates had similar track records with similar recommendations and charisma, I might lean towards going for the gal with the Ivy-league degree, especially if I am running an Ivy-League department.
If I needed a doctor in the private sector, the institution that granted the degree is unlikely going to matter much at all. Yale? Great. Wayne State? That’s okay with me. You just need to be ethical, hard-working, and reasonable to deal with. For all other qualities, the verification process in each state and governing medical board can do the rest.
DO DOCTORS FROM PRESTIGIOUS INSTITUTIONS MAKE MORE MONEY?
It depends again. To understand this question, you should understand how doctors make money to see whether an Ivy-League degree will translate to higher dollars. This is also contingent upon how you are using your medical degree, whether you are practicing medicine, performing administrative work, or consulting. Remember, you don’t have to be a doctor to get rich. Or you shouldn’t become a doctor if your main goal is to become rich.
If we are considering doctor worth from revenue alone obtained through clinical practice, insurance companies make no distinction between where you obtained your degree. U.S. grad, international grad, it doesn’t matter. As long as you pass your boards (sometimes you don’t even have to do that!), you’re golden. From clinical practice alone, you’re not going to make more money having gone to a top college or medical school. Period.
Now having that special degree CAN get you more business, depending on which part of the country you practice medicine. This is particularly true (and sometimes annoyingly so) in the New England area. Patients in New Caanan Connecticut do (in general) care where you obtained your degree. They may or may not even be highly educated, but the high concentration of Ivies in that region predisposes this behavior. Unless you have significant street cred and have been working in the area for a long time, your patient may doctor shop your degree.
OKAY, I SANK $200,000+ INTO AN IVY-LEAGUE MEDICAL DEGREE, WHAT AM I GOING TO GET IN RETURN?
Many of us, under the guidance of family, friends, or schooling, end up enrolling in well-known [read: expensive] private universities and medical schools.
DESPITE the equivocal conclusion by Smart Money MD.
Don’t fret. You’re not totally screwed. If you have a good inheritance coming your way or an alternative means to fund the process, you’re actually in great shape.
If the above doesn’t apply to you, don’t fret either!
STEP 1. PAT YOURSELF ON THE BACK.
Congratulations. It is not easy getting in. It is SIGNIFICANTLY more difficult to get in medical
school than law school, business school, or college. Kudos to you.
This is a fact. By numbers alone. There are simply fewer number of available positions in medical school. The Class of 2018 Stanford Graduate School of Business has 417 new students. Last I checked, the Stanford medical school had fewer than 90 students per class. I think the acceptance rate in the medical school was about 2-3%, while the business school acceptance rate was 6%. If you compare these numbers to that of an average public medical school and public business school, you’ll see that the class sizes will be larger and the acceptance rate will also be higher.
STEP 2. YOU’VE GOT A LIFETIME OF PRESTIGE ATTRIBUTED TO YOUR NAME.
Yup, your mother can brag about her daughter at every holiday party. Your distant relatives will direct their children to you for advice. Your alma mater will also hit you up for donations every single year. You can volunteer with your local alumni group and have “exclusive parties”.
You have a lifetime of memories and connections to potentially successful friends and colleagues.
This is not a bad situation to be in.
STEP 3. CLEAR YOUR MIND AND GET TO WORK.
Get yourself back into the real world. Don’t let anything else cloud your judgment. You’re probably not even that smart. Your coworker at the hospital who came from Portugal probably is one the smartest gals in her country. She memorized Harrison’s twice to pass her country’s exams. Oh yea, she also repeated residency in the U.S. and passed all of her U.S. board exams…in English.
That’s right, her native tongue is Portuguese, and she learned Spanish as her secondary language. English was her third language.
Get yourself out of debt if you funded your education through loan sharks. If I dug myself out of debt, so can you. Save up your money. Figure out how much you are worth.
Figure out what makes you happy. Then work to get there. Easy peasy.
Smart Money MD, an ophthalmologist run financial website, focuses on proper management of medical trainee debt, lifestyle, time, and getting the most out of your hard-earned degree.
I can only second what Smart Money said above. In the grand scheme of things, getting into medical school is a much bigger deal than which medical school you get into. For most residency programs, what you get on USMLE Step 1 will carry much greater weight than your medical school. However, all else being equal, more prestigious medical schools will have more famous faculty, who will be better able to plug you into opportunities to advance your career as well as make phone calls on your behalf when it comes time for Match Day or even beyond with jobs. For more competitive training programs, specialties, or jobs, this may make a huge difference. To decide, ask yourself what type of training and career you want, then find a medical school training program that will you make you happy. Good luck!
Advice on how to succeed in medical school, apply for residency programs, and become a physician
Monday, March 27, 2017
Thursday, March 23, 2017
Age-Appropriate Screening Guidelines
As you encounter patients in a primary care setting, you play an important role in preventative medicine. Specifically, you must ensure that your patients are receiving appropriate screening given their age, gender, and risk factors. Especially after the implementation of the Affordable Care Act, preventive services have taken on an even greater importance.
The main body that puts together guidelines in the United States is the U.S. Preventive Services Task Force, or USPSTF:
The selected guidelines below cover some of the most common recommendations:
Women
Men
Several interesting or unexpected exceptions to screening guidelines exist. For all, there is no specific recommended screening for skin cancer for the general population. That being said, one should still protect themselves from excessive skin exposure and follow up on any unusual skin findings. For men, the USPSTF recommends against screening for testicular and prostate cancer with PSA. For women, no screening for ovarian cancer exists presently. Women who have a strong family history of breast or gynecologic cancers should be screened for BRCA-1/2 and referred for genetic counseling if the tests are positive.
If there are other screening guidelines you feel should be included on here, please comment below or contact me. For more detailed information, check out Current Practice Guidelines in Primary Care for 2017:
The main body that puts together guidelines in the United States is the U.S. Preventive Services Task Force, or USPSTF:
The U.S. Preventive Services Task Force is an independent panel of experts in primary care and prevention who systematically reviews the evidence of effectiveness and develops recommendations for clinical preventive services. These reviews are published as U.S. Preventive Services Task Force recommendations on the Task Force Web site and/or in a peer-reviewed journal.Often, the USPSTF guidelines are complemented by recommendations by specialty societies, such as the American Cancer Society or the American College Radiology. Be careful though: sometimes the guidelines may be contradictory, such as what age to start breast cancer screening with mammography. For a comprehensive list, visit the USPSTF website or download their app.
The selected guidelines below cover some of the most common recommendations:
Women
| Age | Recommendation | Grade | |
|---|---|---|---|
| Puberty - 24 | Chlamydia/Gonorrhea if sexually active | B | |
| 21 - 65 | Pap smear every 3 years (if combined with HPV testing, can be every 5 years after age 30) | A | |
| 40 - 49 | Individual decision for screening mammogram based on relative benefits vs risks | C | |
| 50 - 74 | Biennial screening mammography | B | |
| 50 - 75 | 1) Annual screening with fecal immunochemical test (FIT) 2) screening every 10 years with flexible sigmoidoscopy and annual screening with FIT 3) screening every 10 years with colonoscopy 4) screening every 5 years with CT colonography. |
A | |
| 55 - 80 |
|
B |
Men
| Age | Recommendation | Grade |
|---|---|---|
| 50 - 75 | 1) Annual screening with fecal immunochemical test (FIT) 2) screening every 10 years with flexible sigmoidoscopy and annual screening with FIT 3) screening every 10 years with colonoscopy 4) screening every 5 years with CT colonography. | A |
| 55 - 80 | Low dose lung CT if one has a 30 pack-year smoking history, currently smokes or quit within the last 15 years. | B |
Several interesting or unexpected exceptions to screening guidelines exist. For all, there is no specific recommended screening for skin cancer for the general population. That being said, one should still protect themselves from excessive skin exposure and follow up on any unusual skin findings. For men, the USPSTF recommends against screening for testicular and prostate cancer with PSA. For women, no screening for ovarian cancer exists presently. Women who have a strong family history of breast or gynecologic cancers should be screened for BRCA-1/2 and referred for genetic counseling if the tests are positive.
If there are other screening guidelines you feel should be included on here, please comment below or contact me. For more detailed information, check out Current Practice Guidelines in Primary Care for 2017:
Tuesday, March 21, 2017
Medical School Student Loan Consolidation And Refinancing: A Primer
Today's post is a repost from Future Proof, MD covering the basics of medical student loan consolidation and refinancing:
If you are like the majority of medical school graduates out there, you're probably saddled with a good amount of student debt. I know I am. If you are like me, you may have gathered multiple loans from several different lenders over your many years of schooling. Now that you're finally done with school and entered the workforce, you may have been bombarded with emails inviting you to consolidate/refinance your loans. So let's talk loan consolidation/refinancing.
First, let's address what consolidation and refinancing are.
PROS:
CONS:
For those of you currently in medical school, I would also add that I strongly encourage you to seek out grants, stipends, and scholarships to supplement your financing. There are many tied to specific student backgrounds (i.e., if you come from a minority group), or for those willing to perform public or military service for some time after finishing training. Personally, I can attest to this being a very valuable approach as a single scholarship application that I knocked out one weekend evening ended up covering my tuition for an entire semester! Another example is author Ramit Sethi who funded his entire Stanford undergraduate education on scholarship money alone. If you need a primer on personal finance overall, his NY Times bestselling book I Will Teach You To Be Rich is a great place to start:
If you are like the majority of medical school graduates out there, you're probably saddled with a good amount of student debt. I know I am. If you are like me, you may have gathered multiple loans from several different lenders over your many years of schooling. Now that you're finally done with school and entered the workforce, you may have been bombarded with emails inviting you to consolidate/refinance your loans. So let's talk loan consolidation/refinancing.
First, let's address what consolidation and refinancing are.
- Consolidation allow you to combine multiple loans into 1 loan, resulting in just 1 monthly payment instead of many. For example, if you have only federal loans and go through federal loan consolidation, you will end up with 1 bill but your interest rate will simply be a weighted average of all the different interest rates of the loans you consolidated.
- Refinancing, on the other hand, allow your to consolidate your loans as above. But the difference is that your new interest rate will be dependent on your credit score and history rather than what the interest rates on your old loans were. In essence, you are applying for a new loan with new terms to pay off your old loans - analogous to a "balance transfer" between credit cards. In reality, "consolidation" and "refinancing" are used interchangeably. If you are getting an offer to "consolidate" your loans through a private lender, they're talking about refinancing. For the purpose of our discussion, I will use the term "refinance".
PROS:
- 1 monthly payment. This is probably the biggest benefit of refinancing your loans. Instead of making multiple monthly payments to multiple lenders, you get 1 bill and 1 payment.
- You may qualify for a lower interest rate. The standard interest rate for federal student loans are fixed at 6.8%. If you have good credit and income, it's likely you will qualify for a lower interest rate. I say "may" because when I went through SoFi (the largest student loan refinancing lender) to check what they would do for me, my refinancing offer was less than generous (see figure).
- You can lower your monthly payment. This can result from you getting a lower interest rate on the new loan, by renegotiating your repayment term (15 or 20 years instead of the standard 10 years for a standard repayment plan), or a combination of both.
- Choice of variable vs. fixed interest rates. Choosing a variable interest rate will benefit those who are planning to pay off their student loans rapidly.
CONS:
- Refinancing your loans with a private lender will make you ineligible for federal loan forgiveness programs such as Public Service Loan Forgiveness (PSLF), and other benefits such as Income Based Repayment (IBR), deferments and forbearance.
- Your interest rate may go up if you choose a variable interest rate plan. Most variable interest rate loans have a cap as to how high the interest rate can reach, but it's usually more than the standard 6.8% fixed you would get through the government.
- It's a permanent decision - if you ever leave the federal system, there is no recourse if you decide later that you've made a mistake.
- Fees - this is a minor consideration for those with a large loan balance, but there may be fees associated with a private loan refinancing application.
- So after considering many of the above factors, I ended up consolidating my loans through the government. I am currently on Income Based Repayment (IBR) with plans to eventually qualify for Public Service Loan Forgiveness.
For those of you currently in medical school, I would also add that I strongly encourage you to seek out grants, stipends, and scholarships to supplement your financing. There are many tied to specific student backgrounds (i.e., if you come from a minority group), or for those willing to perform public or military service for some time after finishing training. Personally, I can attest to this being a very valuable approach as a single scholarship application that I knocked out one weekend evening ended up covering my tuition for an entire semester! Another example is author Ramit Sethi who funded his entire Stanford undergraduate education on scholarship money alone. If you need a primer on personal finance overall, his NY Times bestselling book I Will Teach You To Be Rich is a great place to start:
Friday, March 17, 2017
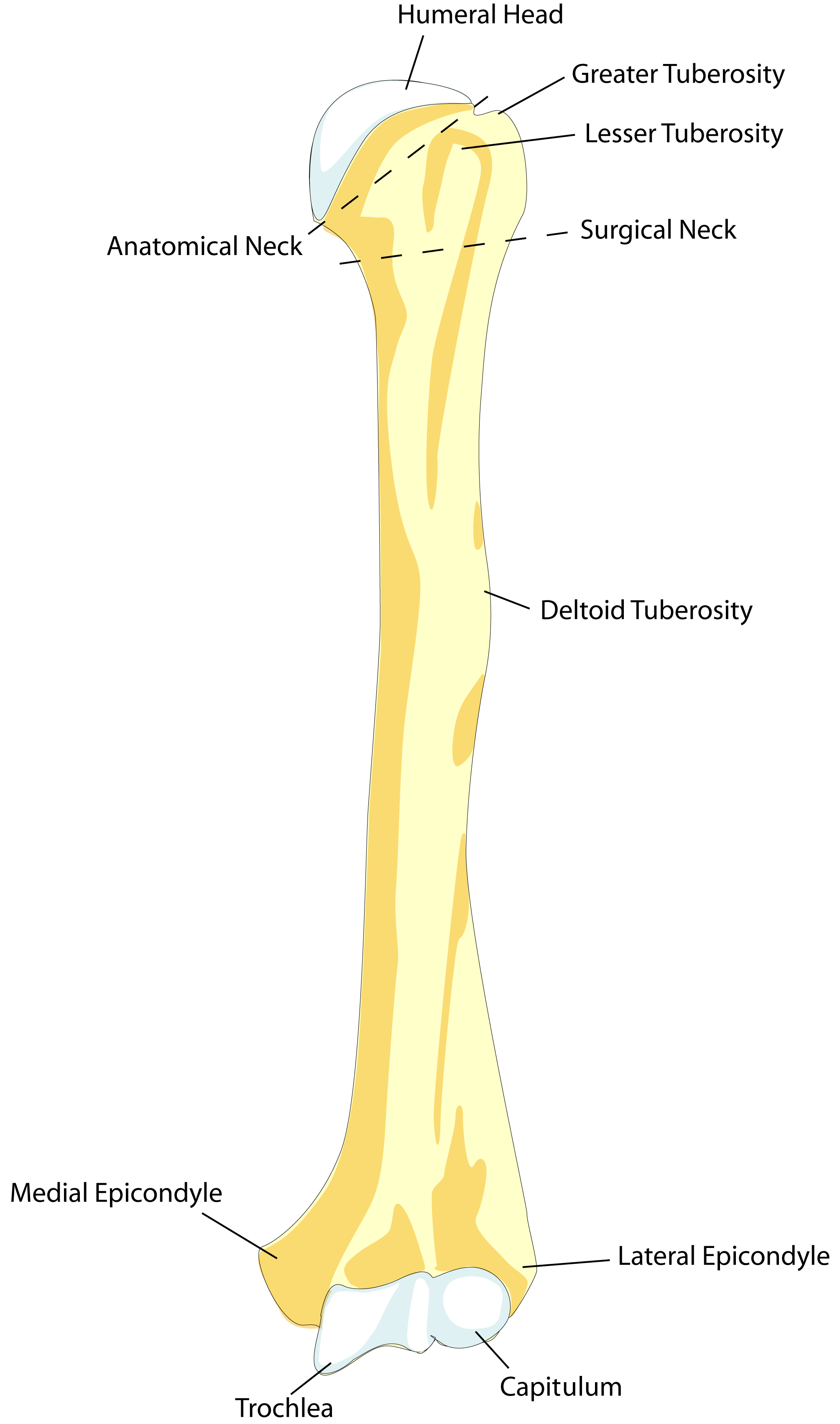
Humerus Anatomic Neck vs. Humerus Surgical Neck
One of the most popular posts on this site was a deep dive into the difference between Pope's Blessing and Claw Hand. Who knew anatomy could be so contentious? Admittedly, today's post is likely much less controversial, but I always found the distinction between the anatomic neck of the humerus and the surgical neck of the humerus to be confusing. Well, prepare yourself for today's shallow dive into the subject. Hopefully this will help clarify the distinction between the two. If it's already clear to you, congratulations - at least one of us will benefit from this exercise!
The anatomic neck of the humerus refers to the location of the physeal plate during development. During growth, bone forms at the physeal plate as the child ages. Once the child reaches maturity, the plate closes, usually during puberty. Different growth plates will close at different ages, with well-characterized ranges known for various bony structures. This pattern of plate closure can be used to assess a child's bone age, which can then be compared to their chronological age to assess for any delay in maturation. Returning to the humerus, the anatomic neck is mostly notable as a defined landmark but has less clinical application.
The surgical neck of the humerus refers to the narrowing of the humerus in the proximal diaphysis. The neck abuts the quadrangular space, a potential space formed by the margins of the triceps, teres minor, teres major, and the medial humerus margin (3 Ts + H, as opposed to the more medial triangular space formed by those same 3 Ts, but no H). Since this region is more prone to fracture, that means fractures in this area are more likely to damage the contents of the quadrangular space, namely the axillary nerve and posterior humeral circumflex artery.
To memorize the difference between the two, you can try a few different ways. First, A for anatomic comes before S for surgical, and the anatomic neck is more proximal on the humerus than the surgical neck. Second, the surgical neck is more often fractured and more likely to have surgical complications, so the name is associated with its clinical relevance.
And that's pretty much it! For me, learning anatomy was much more helpful when I could attach a narrative about some clinical situation in which that anatomy was relevant. Start with a basic framework of the location from a book like Netter's Anatomy and then search for clinical scenarios that help solidify the terminology in your mind. Hope this helps!
The anatomic neck of the humerus refers to the location of the physeal plate during development. During growth, bone forms at the physeal plate as the child ages. Once the child reaches maturity, the plate closes, usually during puberty. Different growth plates will close at different ages, with well-characterized ranges known for various bony structures. This pattern of plate closure can be used to assess a child's bone age, which can then be compared to their chronological age to assess for any delay in maturation. Returning to the humerus, the anatomic neck is mostly notable as a defined landmark but has less clinical application.
The surgical neck of the humerus refers to the narrowing of the humerus in the proximal diaphysis. The neck abuts the quadrangular space, a potential space formed by the margins of the triceps, teres minor, teres major, and the medial humerus margin (3 Ts + H, as opposed to the more medial triangular space formed by those same 3 Ts, but no H). Since this region is more prone to fracture, that means fractures in this area are more likely to damage the contents of the quadrangular space, namely the axillary nerve and posterior humeral circumflex artery.
 |
| By BDB - You can find the picture here. Traced and colored the picture using adobe illustrator., Public Domain, Link |
To memorize the difference between the two, you can try a few different ways. First, A for anatomic comes before S for surgical, and the anatomic neck is more proximal on the humerus than the surgical neck. Second, the surgical neck is more often fractured and more likely to have surgical complications, so the name is associated with its clinical relevance.
And that's pretty much it! For me, learning anatomy was much more helpful when I could attach a narrative about some clinical situation in which that anatomy was relevant. Start with a basic framework of the location from a book like Netter's Anatomy and then search for clinical scenarios that help solidify the terminology in your mind. Hope this helps!
Wednesday, March 15, 2017
ACGME Increases Shift Length For Interns
The American Council of Graduate Medical Education, or ACGME, recently announced that it was reversing course and lengthening the longest shift an intern can work in a hospital from 16 to 24 hours. The ACGME governs the structure of all accredited residency training in the United States, so this change will have broad-ranging effects. While PGY-2 residents and above were already allowed to work these longer shifts, interns had been protected from them since 2010. Here are various summary articles:
However, since 2010, concerns have arisen that the shortened shift actually detracts from intern training as they are required to hand off patients frequently in order to abide by the 16-hour restriction. Often times, a complex patient may require care past the 16 hour mark, which the trainee could not participate in while still complying with the rule.
Another concern was the hand-offs themselves. Especially in July, interns are still learning how to manage patients on a very basic level. Asking them to hand off a complex patient to another intern at the same early training stage is a recipe for error, since clinically relevant information may be omitted or underplayed, leading to errors in the provision of care.
Ostensibly, the ACGME attributes its change to the following reasons:
There have been several minor revisions since 2003, including the move to the 16 hour intern limit in 2010. The debate will continue over striking the appropriate balance between clinical exposure and the physician's personal health. As a medical student, you should inquire with prospective training programs about how they plan to manage the change, as well as ask current program trainees how the program actually functions. In more demanding specialties, such as neurosurgery or orthopedics, there are many programs that have trainees working longer than the hours they actually log. Ultimately, the ACGME is not an enforcing body and cannot assess whether each resident actually works the number of hours they say they do, so it is up to you to ensure the training program you join matches your expectations.
Regardless of whether you join a relaxed program or a stressful one, your best bet to make sure you are as prepared as possible to handle patients clinically on your own. Despite different specialties, intern experiences have a lot of overlap. The following resources below should help you be better prepared for the first day when you round by yourself as a full MD:
Good luck! If you are or recently were an intern, what was your experience like? What do you think of the proposed changes?
However, since 2010, concerns have arisen that the shortened shift actually detracts from intern training as they are required to hand off patients frequently in order to abide by the 16-hour restriction. Often times, a complex patient may require care past the 16 hour mark, which the trainee could not participate in while still complying with the rule.
Another concern was the hand-offs themselves. Especially in July, interns are still learning how to manage patients on a very basic level. Asking them to hand off a complex patient to another intern at the same early training stage is a recipe for error, since clinically relevant information may be omitted or underplayed, leading to errors in the provision of care.
Ostensibly, the ACGME attributes its change to the following reasons:
In keeping with this philosophy, the changes are supported by testimony from a wide range of physician specialty educators and intended to:The trade-off though is a return to the era of the over-worked, fatigued intern. Historically, residency was a brutal training process with no restrictions. The first attempt to curb work hours was set in motion by the death of Libby Zion, an 18 year old girl who was under the care of minimally supervised, overworked trainees. Her father Sidney's anger at her death led to the ACGME instituting its first series of work hour reforms. Even those changes were slow to come around: the commission formed after Zion's death recommended changes including an 80 hour work week restriction in 1989; the ACGME instituted those changes in 2003, fourteen years later.
- place greater emphasis on patient safety and quality improvement;
- more comprehensively address physician well-being;
- strengthen expectations around team-based care; and,
These revisions were developed as part of the ACGME’s periodic review of all program requirements to ensure that professional preparation of physicians adequately addresses the evolving and growing needs of patients.
- create flexibility for programs to schedule clinical and educational work hours within the maximums currently utilized in the US.
There have been several minor revisions since 2003, including the move to the 16 hour intern limit in 2010. The debate will continue over striking the appropriate balance between clinical exposure and the physician's personal health. As a medical student, you should inquire with prospective training programs about how they plan to manage the change, as well as ask current program trainees how the program actually functions. In more demanding specialties, such as neurosurgery or orthopedics, there are many programs that have trainees working longer than the hours they actually log. Ultimately, the ACGME is not an enforcing body and cannot assess whether each resident actually works the number of hours they say they do, so it is up to you to ensure the training program you join matches your expectations.
Regardless of whether you join a relaxed program or a stressful one, your best bet to make sure you are as prepared as possible to handle patients clinically on your own. Despite different specialties, intern experiences have a lot of overlap. The following resources below should help you be better prepared for the first day when you round by yourself as a full MD:
- Pocket Medicine by Marc S. Sabatine
A handy guide that easily fits into a white coat pocket, Pocket Medicine has long been essential reading for interns, especially those on medicine wards. This small book is chock full of practical tips and broad differentials for common clinic findings. - First Aid for the Wards by Tao Le, Vikas Bhushan, et al.
From the authors of First Aid for USMLE Step 1, the bible of Step 1 prep, comes this book about rotation-specific advice. While intended for MS3 students, it still contains lots of useful information for interns, especially those who will rotate among various specialties, such as transitional interns. - Intern by Sandeep Jauhar
While not a technical guide like the two prior books, this memoir by Dr. Jauhar gives a good sense of what it feels like to be an intern, especially the sense of disorientation one may feel at times.
Good luck! If you are or recently were an intern, what was your experience like? What do you think of the proposed changes?
Tuesday, March 14, 2017
Amazon Fire Tablet Deal
We have previously written about tablets for medical students, and why you might want one. If you're not sold on a top of the iPad Pro, consider this deal for an Amazon Fire Tablet Essentials Bundle (16GB):
Simply enter the code FIREBUNDLE at check out and get the 16GB version, case, and a screen protector for less than you would spend for the tablet itself. If you do get any kind of tablet, a case or cover is a must. Think about it: between carrying it to and from the classroom, library, or wards, the various fluids and substances in a healthcare setting, and the possibility of others using it, the tablet is prone to falls. As we discussed recently, you should also consider the pros and cons of getting a warranty.
In addition to a case, you should consider a Bluetooth keyboard. I'm personally a huge fan of the Kensington keyboard/case combo I got for my iPad Air 2, the Kensington Key Folio Thin X3:
It works great, is backlit, and last for almost a solid *year* on a single charge via microUSB. It has proven invaluable for taking notes and making the device more functional. The combination practically serves as a laptop replacement for most light to moderate computing tasks. Not to mention weighing a ton less! For any medical student with limited carrying / storage space, such a compact solution is a definite plus.
In addition to a case, you should consider a Bluetooth keyboard. I'm personally a huge fan of the Kensington keyboard/case combo I got for my iPad Air 2, the Kensington Key Folio Thin X3:
It works great, is backlit, and last for almost a solid *year* on a single charge via microUSB. It has proven invaluable for taking notes and making the device more functional. The combination practically serves as a laptop replacement for most light to moderate computing tasks. Not to mention weighing a ton less! For any medical student with limited carrying / storage space, such a compact solution is a definite plus.
Subscribe to:
Posts (Atom)